1202
Nurse Liaison and Educator Meridian at Home Hospice
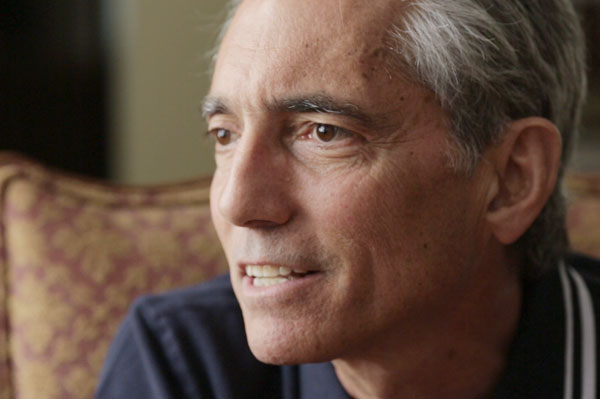
Anne Marie McLaughlin, RN, BSN, BA, CHPN
Anne Marie has been a nurse for 8 years, and is currently pursuing her graduate degree. In her work, she has often served as a bridge between the hospital setting and hospice, helping patients transition from one to the other. She feels strongly that nurses can change the cultural tide with doctors, patients and their families to embrace palliative care sooner in the disease process, whether it be a cancer diagnosis or something more long term, such as early stage Alzheimer's or COPD.
https://www.dyinginamerica.org/wp-content/uploads/2015/08/C1_5416web1-549x366.jpg